The latest research from ANSIRH supports the safety and effectiveness of prescribing abortion pills without a screening pelvic exam or ultrasound, enabling more access to abortion care.
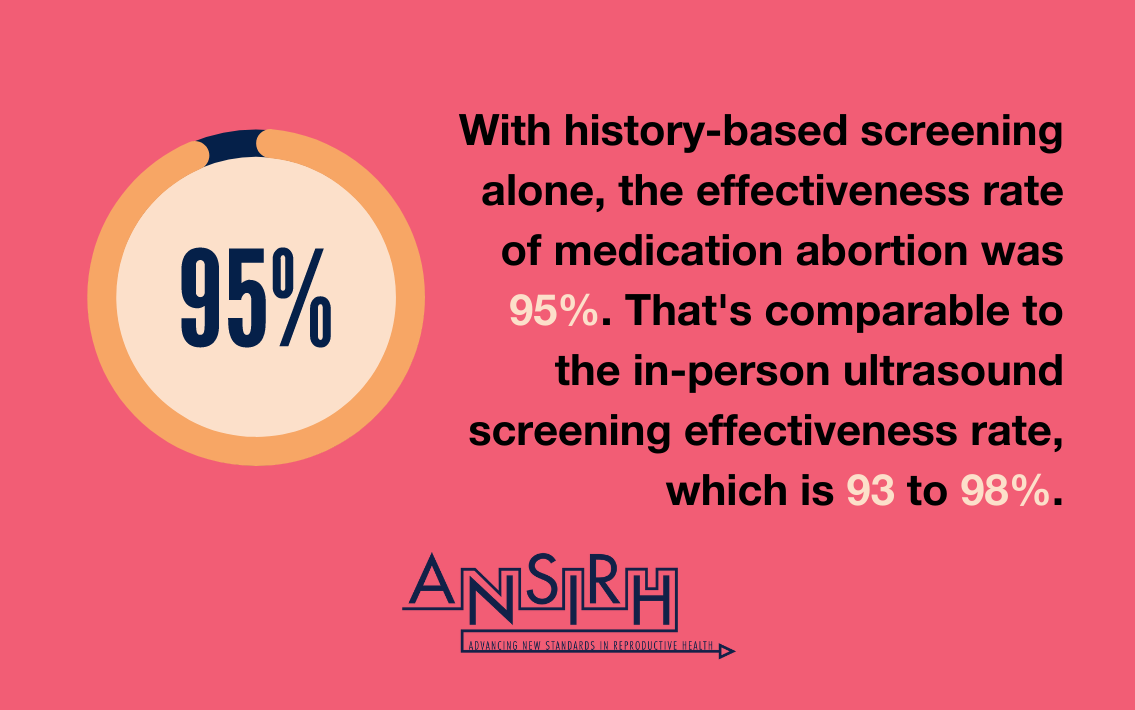
Screening for medication abortion typically has included in-person examination with an ultrasound or pelvic exam, though several states have enacted mandatory ultrasound laws that are not medically necessary. Many providers stopped requiring these tests to reduce physical contact during the COVID-19 pandemic and instead screened patients by medical history alone. We sought to evaluate this updated model of care for effectiveness and safety.
Key Findings
Study Design
- Study population: 3,779 eligible abortions
- Characteristics: Patients were diverse, majority being Black, Indigenous, or people of color, and half paid for the abortion—at least in-part—out of pocket.
- Geography: 34 states, mostly in urban areas
- Additional data: For 66.4% of abortions, the medications were dispensed in person and for 33.6%, they were mailed to the patient.
Implications
History-based screening alone for medication abortion eligibility is safe and effective, and this new process could increase the number of physicians and nurse practitioners providing medication abortion in the U.S. With the possibility of the Supreme Court overturning Roe V. Wade this year, and an increasing number of gestational bans, it will become especially crucial for state public health efforts to reduce logistical, distance, and cost barriers to abortion. Medication abortion eligibility based on patient history can lower these costs, reach marginalized patients, and allow patients to avoid harassment at clinics, with outcomes similar to models of in-person care.
The researchers write:
“These benefits have the potential to increase equitable access for all abortion patients, particularly people of color, low-income people, rural people, and those who face greater barriers to abortion care. Clinicians should eliminate unnecessary tests to support patient-centered care.”
The article, Outcomes and Safety of History-Based Screening for Medication Abortion: A Retrospective Multicenter Cohort Study, is available in JAMA Internal Medicine.
